Bioactive glass has gained significant attention in dental implants due to its unique properties like osteoconductive and osteo-stimulatory characteristics, along with its superior biocompatibility making it a promising material for use in dentistry. Here is an overview of the role and potential benefits of bioactive glass as a replacement or component in dental implants:
Osteoconduction and Bone Regeneration
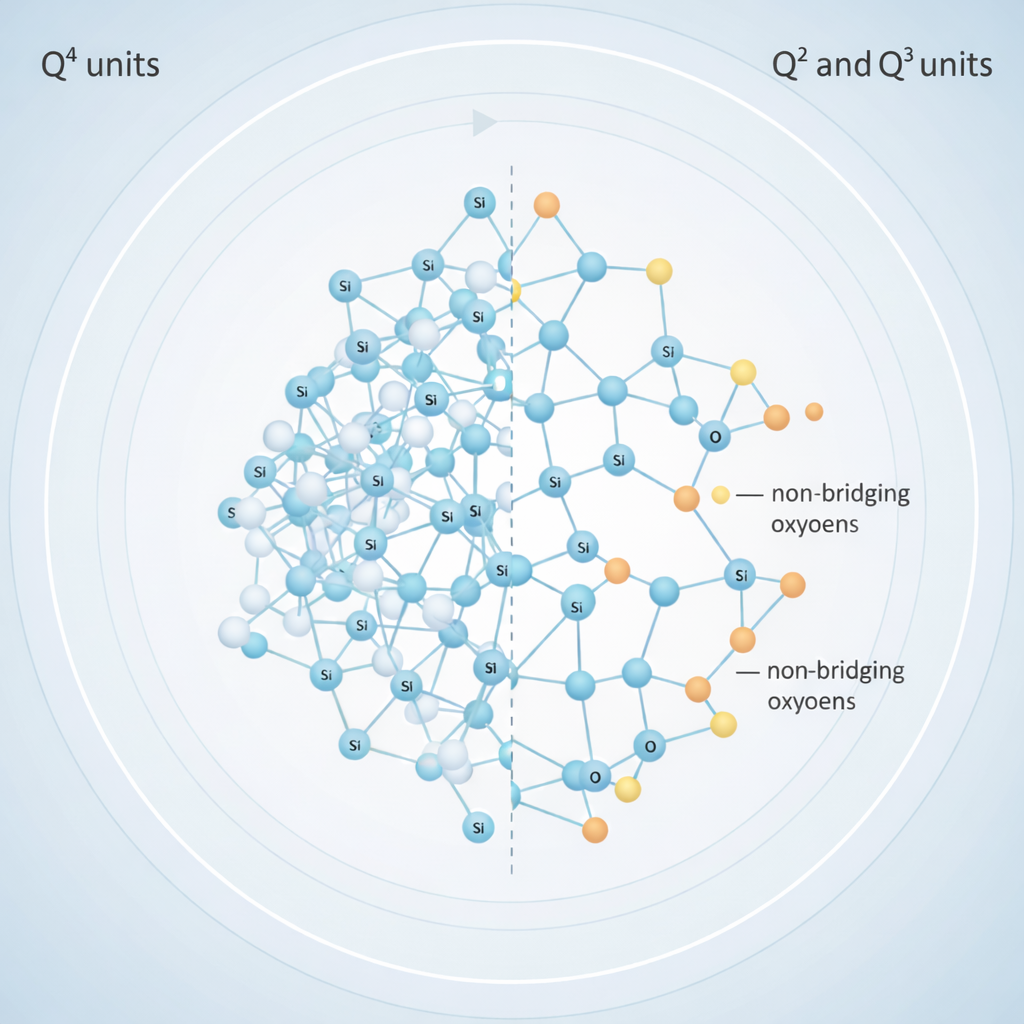
Bioactive glass is a material that is known to be osteoconductive due to its capacity to form bonds with both soft tissue and bone. By promoting the formation of new bone surrounding the implant, it improves the osseointegration process. The substance releases calcium, phosphate, and silicon ions that promote the production of hydroxyapatite (HA), a valuable component of bone that is a mineral form of calcium phosphate. The healing process and long-term viability of dental implants are enhanced by this characteristic.
The material leaches ionic components, such as calcium (Ca²⁺), phosphates (PO₄³⁻), and silicon (SiO₄⁴⁻), which stimulate local cells to enhance osteogenic differentiation. This can further promote bone healing, even in areas where bone density is low, or in cases where additional stimulation is required for bone regeneration.
Bioactive interaction with tissue
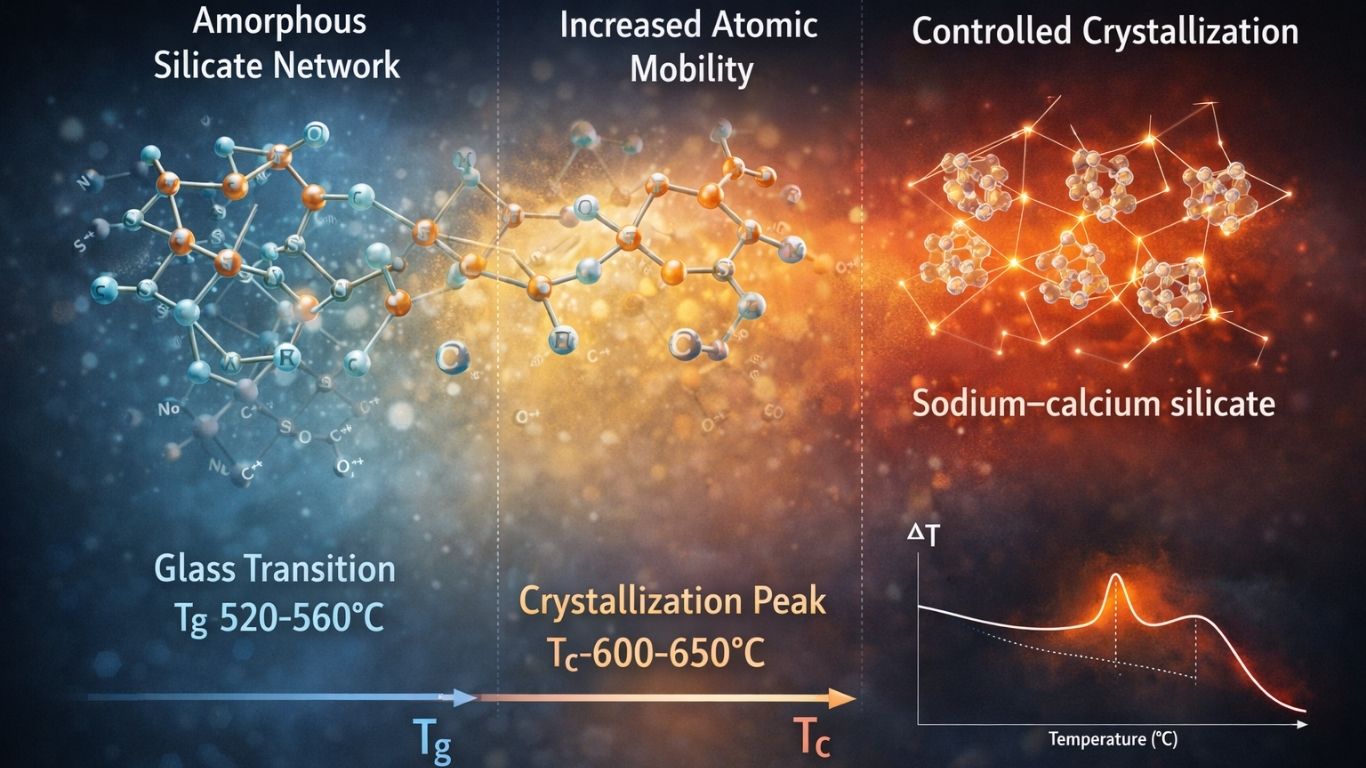
The surface reactivity of bioactive glass gives it a special ability to adhere firmly to soft tissue and bone. After being inserted, it reacts on the surface with bodily fluids to create a layer that resembles real bone. This bioactive reaction speeds up the implant’s integration into the bone by encouraging tissue regeneration and healing.
In traditional implants, the implant placement might require more significant incisions. In contrast, bioactive glass implants require less disruption of the surrounding tissue, leading to a reduced need for suturing, less swelling, and a quicker recovery for the patient.

Promoting long term implant stability
The bioactivity of the glass leads to the formation of a strong bond with the surrounding bone, providing mechanical support and stability to the dental implant. This can improve the longevity of the implant, as bioactive glass helps to distribute mechanical forces evenly across the implant and surrounding tissues, reducing the risk of implant failure due to stress or micromotion. The healing process is often faster and more efficient compared to traditional methods that might require larger grafts or additional surgeries to augment bone volume.
Reduction of foreign body response
Bioactive glasses react with the body’s biological fluids to form a bioactive surface that mimics the natural mineral content of bone. This forms a strong bond with the surrounding bone and soft tissues, which helps prevent the immune system from recognizing the material as a foreign body. The surface of bioactive glass is chemically active, promoting the formation of a hydroxyapatite layer similar to the mineral structure found in bones, facilitating integration rather than rejection. This reduces the severity of the inflammatory response that can occur with non-bioactive materials.
Aesthetic Advantages
The aesthetic advantages of bioactive glass in dental implants primarily lie in its ability to mimic the natural look of teeth, providing a translucent, smooth, and natural appearance. It also avoids common aesthetic concerns seen with metal implants, such as gum discoloration and tarnishing, while enhancing the integration between the implant and surrounding tissues. These benefits make bioactive glass an excellent choice for patients seeking both functional and aesthetic outcomes in dental restoration.
Less Invasive Surgical Approach
By encouraging quicker osseointegration, requiring fewer incisions, and minimizing the need for bone grafting or extensive soft tissue manipulation, bioactive glass makes a less invasive surgical approach possible. The material’s biocompatibility, capacity to adhere to soft tissues and bone, and capacity to promote natural healing all help patients recover more quickly and comfortably. Because of this, bioactive glass is a good choice for patients looking for a minimally invasive dental implant procedure that has great long-term results.
Challenges with Bioactive glass
1. Mechanical Strength and Brittleness
Bioactive glass, particularly in its pure form, tends to be more brittle compared to traditional materials like titanium or ceramics. This brittleness limits its use in applications where high mechanical strength is required, such as in load-bearingareas of the body, or in dental implants subjected to chewing forces.
To overcome this, bioactive glass is often used in combination with other materials (e.g., titanium alloys, composite materials) to enhance its mechanical properties. Additionally, composite forms of bioactive glass are being developed to increase toughness without compromising its bioactive capabilities.
2. Limited commercial availability
While bioactive glass has shown great promise, its widespread commercial availability for dental and orthopaedic applications is still limited compared to established materials like titanium. This limitation is partly due to the material’s cost, manufacturing challenges, and the need for more clinical validation.
Conclusion:
Bioactive glass represents a promising alternative or complementary material in dental implants, offering benefits in terms of osseointegration, bone regeneration, and overall implant stability. However, its application must be carefully considered in terms of strength, long-term performance, and cost.
The superior biocompatibility of bioactive glass makes it an ideal material for integration with both bone and soft tissues, minimizing the risk of rejection and complications. This makes Bioactive glass a promising material for enhancing implant success rates, improving bone healing, and reducing invasive surgical interventions.