Bioactive glass (BG) is a synthetic biomaterial renowned for its unique ability to interact with biological tissues and promote regeneration, especially in bone repair applications. This material is not just a scaffold; it’s an active participant in the healing process.
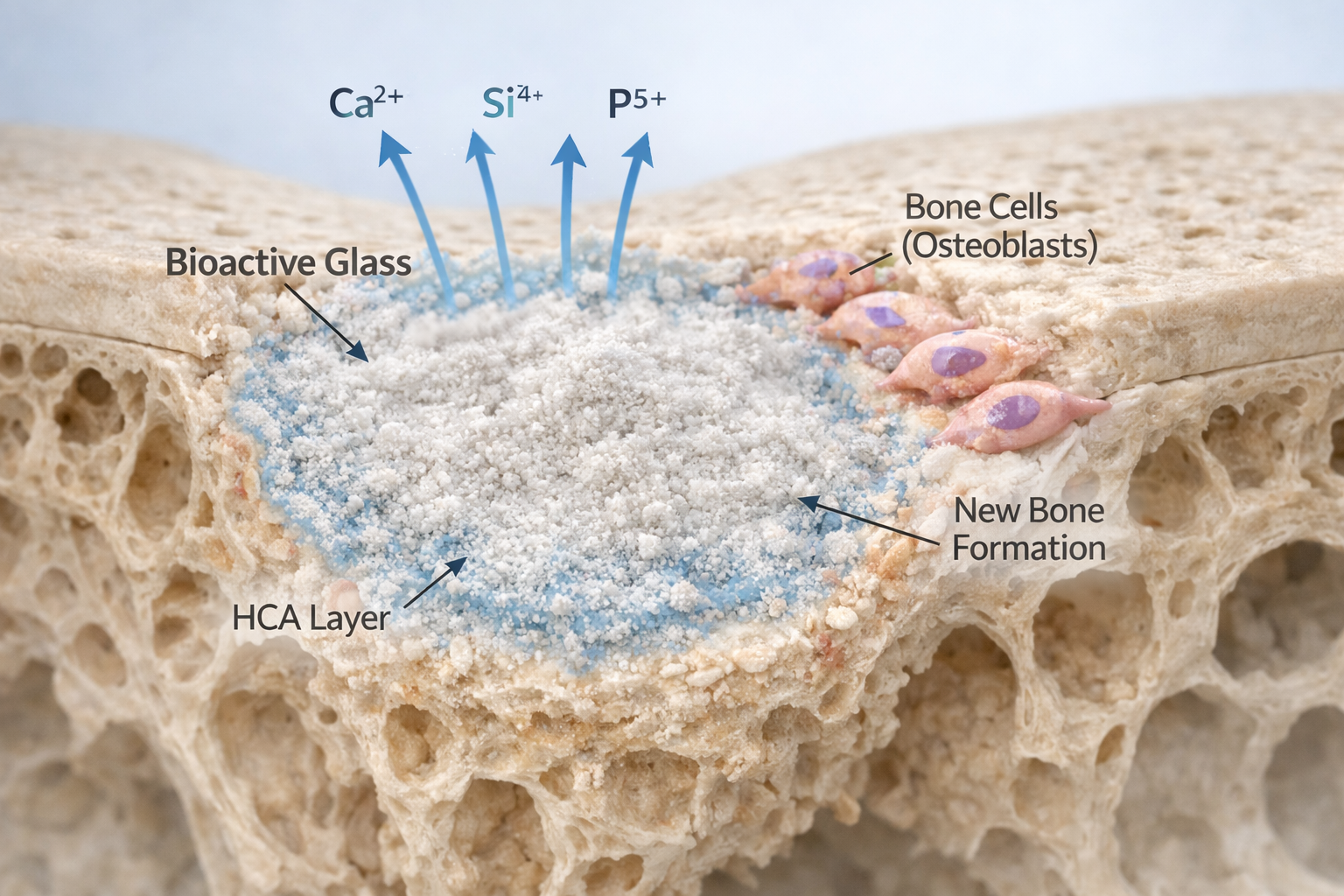
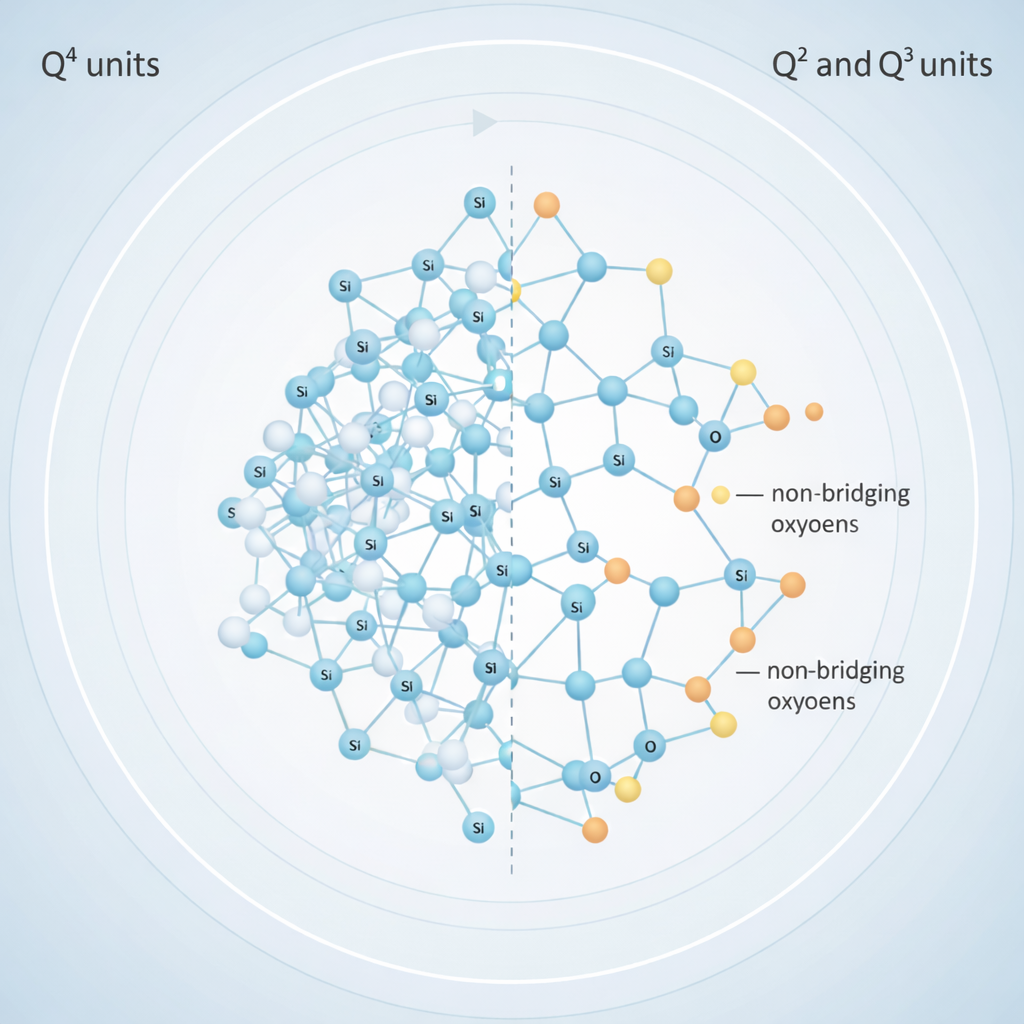
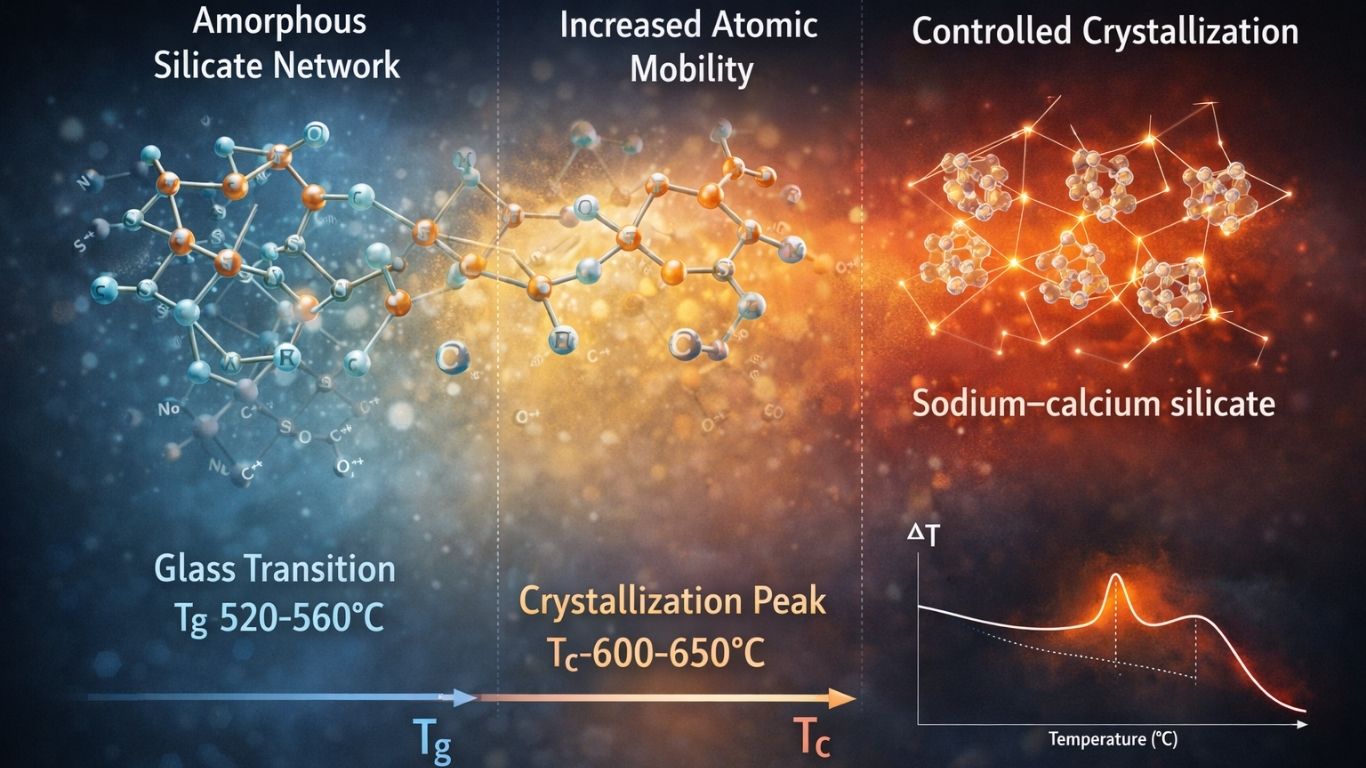
Its unique composition, typically including silicon dioxide, calcium oxide, sodium oxide, and phosphorus pentoxide (with the 45S5 Bioglass® formulation being the most studied), allows it to mimic the body’s natural bone mineral. When immersed in physiological fluids, bioactive glass forms a hydroxycarbonate apatite (HCA) layer, creating a strong, chemical bond with surrounding tissue. Beyond this structural benefit, the material releases key ionic dissolution products—such as calcium, phosphate, and silicon ions—that act as crucial biochemical signals. These ions stimulate cell adhesion, proliferation, and, most importantly, differentiation, making bioactive glass an unparalleled candidate for tissue engineering scaffolds (1).
Synergistic Regeneration: Bioactive Glass and Mesenchymal Stem Cells

To unlock the full regenerative potential of BG, researchers commonly employ Mesenchymal Stem Cells (MSCs). MSCs are multipotent cells capable of differentiating into various cell lineages, including osteoblasts (bone-forming cells).
The combination is powerful:
Structural Support: The bioactive glass scaffold provides a three-dimensional, porous framework for MSC attachment and migration.
Active Stimulation: The scaffold actively stimulates osteogenesis by releasing bioactive ions, creating an optimal environment that closely mimics the natural extracellular matrix (2).
In culture, this synergy encourages MSCs to proliferate and differentiate into bone-forming cells. Researchers often supplement the culture medium with specific osteogenic factors (like dexamethasone) to further accelerate the process. The resulting increase in cell viability and enhanced expression of osteogenic markers like alkaline phosphatase (ALP), osteocalcin (OCN), and RUNX2 confirms successful bone-like tissue formation (3).
How is Stem Cell Differentiation on Bioactive Glass Measured?
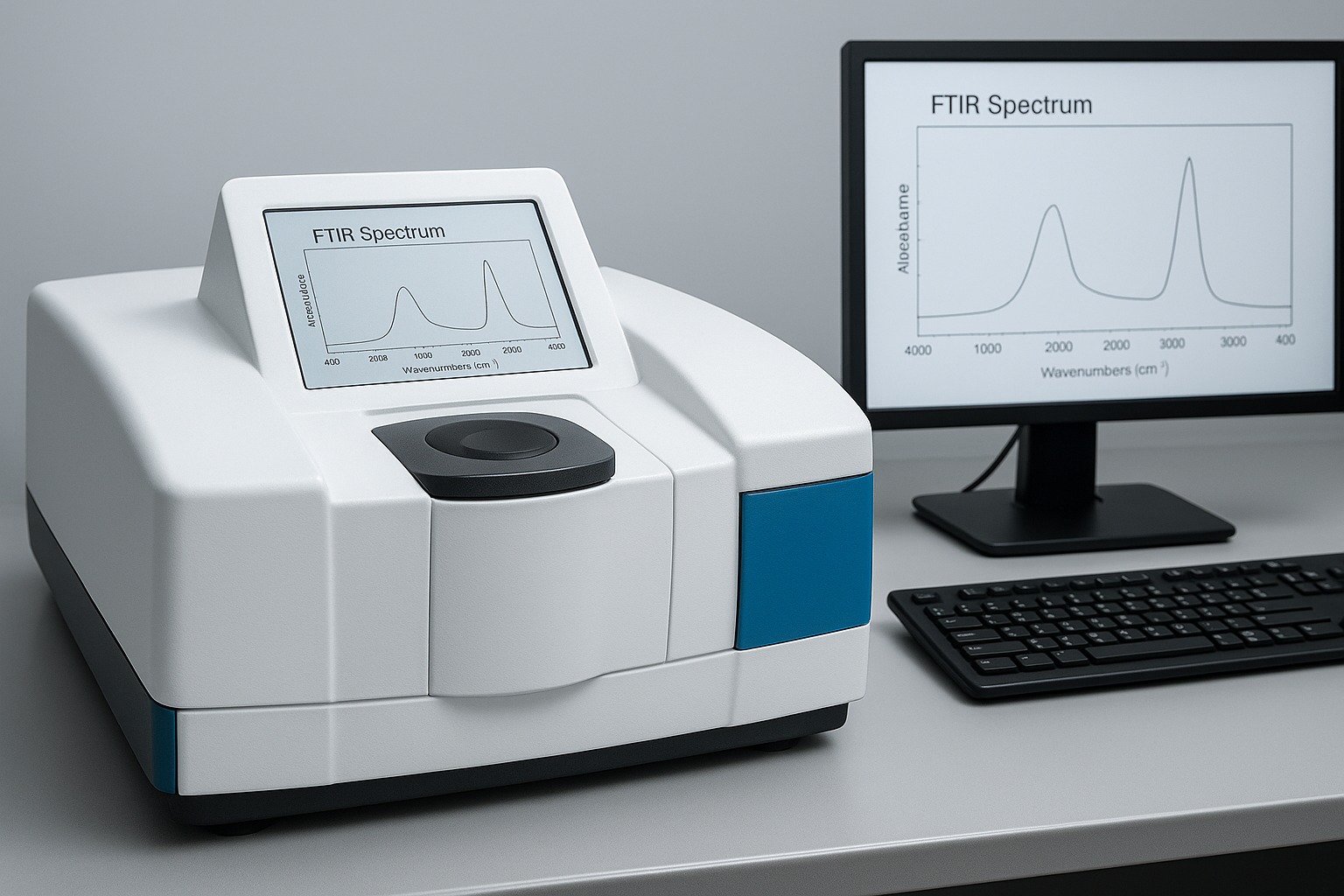
To validate the efficacy of bioactive glass in promoting functional tissue regeneration, researchers employ a multi-dimensional approach utilizing molecular, biochemical, and histological techniques.
Molecular Analysis: Tracking Gene Expression
The first step in assessing differentiation is often gene expression analysis via quantitative real-time polymerase chain reaction (qPCR). By quantifying the expression levels of key differentiation-related genes, researchers gain insights into the transcriptional changes driven by the bioactive environment.
Osteogenesis Markers: Upregulation of Runx2, ALP, COL1A1 (collagen type I), and OCN over time is a clear indication that the bioactive glass is pushing the stem cells toward an osteoblastic lineage (5).
Other Markers: SOX9, aggrecan (for chondrogenic differentiation), or Nestin/MAP2 (for neurogenic differentiation) are monitored depending on the desired outcome.
Biochemical Verification: Quantifying Proteins
Gene expression must translate into functional protein synthesis. Protein assays confirm this outcome:
Western Blotting: Used to detect and quantify intracellular proteins such as ALP, osteopontin (OPN), and osteocalcin, verifying that differentiation-related proteins are being synthesized (6, 7).
ELISA & Functional Assays: ELISA measures secreted proteins (e.g., VEGF or osteocalcin) in the culture medium. ALP activity assays provide a functional readout of early osteoblastic activity (8).
Histological Assessment: Visualizing New Tissue
The final, compelling evidence of successful differentiation comes from histochemical staining, which visually and spatially assesses matrix production and mineralization—the hallmarks of new tissue formation.
Mineralization Assays: Alizarin Red S staining detects calcium-rich deposits (red color) formed during osteogenesis. Von Kossa staining detects phosphate deposition (dark brown/black areas).
Enzyme Localization: Alkaline phosphatase staining localizes ALP enzyme activity, often appearing as blue or purple regions within the cells.
Immunohistochemistry (IHC): Uses antibodies to localize specific proteins like collagen type I or osteocalcin within the newly formed matrix.
Future Applications and Challenges
The synergy between stem cells and bioactive glass holds immense promise for applications in bone tissue engineering and dental repair. Scaffolds seeded with stem cells can be directly implanted into bone defects, providing structural support while actively promoting new bone growth (4).
However, challenges remain: controlling the rate of ion release to prevent toxicity, ensuring the mechanical integrity of the scaffold for load-bearing applications, and standardizing cell culture protocols are key areas of ongoing research.
Contact us through Synthera Biomedical social platforms to stay informed about pioneering bioactive glass research and clinical applications. Follow us on Instagram for product launches and research updates. Join the conversation on Facebook to access valuable resources and community news.